By James J. O’Mailia, M.D., Gastroenterologist
Two days prior to Thanksgiving, 2008, I developed a sudden onset of severe cramping abdominal pain lasting 2-3 hours, followed by multiple watery bowel movements, and then a few hours later – a complete bowel obstruction needing a surgical resection. There went Thanksgiving dinner! I was diagnosed with a benign (non-cancerous) stricture from recurrent Diverticulitis. This is basically a “strangulation” of the colon, similar to a circular “snag” of a nylon stocking. I had never been ill in my entire life, aside from the flu. To this date, I am the strangest case of Diverticulitis I have ever seen, and certainly not a text-book example.
To begin with, the physiology of the colon is as follows. When the small intestine is finished absorbing the nutrition that you’ve eaten, it flows as liquid stool into the large intestine (colon) on the right side where the appendix is located. The role of the colon is simple – it absorbs the water from the liquid waste. As it approaches the left side of the colon, the stool progressively gets more solid. The left side of the colon is considered the “pump” of the bowel and “squeezes” the solid waste, propelling it as a bowel movement.
If the liquid waste has flowed too slowly, too much water is removed and a hard pebble-like stool develops – constipation. If it flows too fast, an inadequate amount of water is removed and stool remains liquid – diarrhea. That’s the physiology of the colon, in a nutshell.
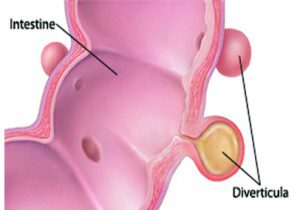
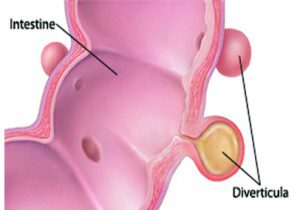
Now, Diverticulitis develops as one might think – mostly on the left side or “pump” side of the colon, where the squeezing of solid-forming waste causes the greatest amount of pressure. Although Diverticulitis can be seen on the right side of the colon, it is not as common. In the colon, there can be weak spots on the specialized colon walls. Due to increased pressure, these weak spots develop sacks or pouches, like bubble forming on an old inner-tube. These pouches are called “diverticula”, or singular – “diverticulum”. As a group, the pouches are called Diverticulosis, and when they are inflamed – Diverticulitis. An analogy would be a head (diverticulum) and a headache (Diverticulitis ).
Ok, so who gets Diverticulosis? Generally, as it takes years to develop, it is seen in an older adult population. This varies greatly, as I have seen this condition in some adults in their late 20’s and early 30’s – presenting first as painful Diverticulitis . I am sure, though, that there have been cases at even younger ages. Diverticulosis develops because we are, for the most part, a low-fiber society. In other words, a meat and potatoes Western society. Asians and Africans rarely experience this problem due to the difference in their diets compared to ours.
As for the more “typical” symptoms of Diverticulitis, patients can experience an intermittent dull or crampy pain located on the left side of the colon and is as-
sociated with progressing constipation. In a more advanced and extensive condition of Diverticulosis, the bowel can become very narrowed, and tortuous or twisted – leading to a change in bowel habits, a pencil-caliber of stool, or constipation followed by a rush of diarrhea.
Of course, these symptoms can be common in other non-diverticulosis presentations, such as Irritable Bowel Syndrome (IBS). When [normal] bacteria seeps from the intestine into the diverticula (pouches), then pressure in the colon – from constipation or, in some cases, diarrhea – can cause the pouches to rupture, thereby creating an opening in the intestinal wall. Stool can rush into the peritoneal cavity, causing acute pain or Diverticulitis, not to mention a host of other medical issues. Thankfully, most cases – around 75% – are self-limited and are treated with bowel rest and antibiotics. In some cases, a short hospital stay is needed.
In few cases, the rupture is large; an abscess (pocket of pus) can develop, which can lead to surgery for a partial resection of the diseased colon. In its most severe presentation, a colostomy or external “bag” is needed. More rarely, rectal bleeding is the presentation. Often, it is not associated with pain and can lead to multiple bloody bowel movements in the span of a few hours. Although this always alarms patients, it generally is treated with a short hospital stay and resolves on its own, sometimes with the need for blood transfusions. In my 30 years of practice, and thousands of Diverticulitis cases, I can count on two hands how many have needed emergent surgery.
Diagnostically, Diverticulosis is discovered with colonscopy or noted routinely on some xrays. However, the quantity of diverticula needed to define the severity of Diverticulitis is not helpful in treatment or prevention. Certainly, the more advanced the quantity or twisting/narrowing of the colon, the greater the risk of rupture. I have found that the key to preventing Diverticulitis is to make sure you are having relatively normal bowel movements – ie, tube-like, soft (not mushy), solid (not hard or pebble-like) stools. Your doctor, particularly, your gastroenterologist, can help you tailor your diet to your needs.
Finally, let me put an old myth to rest. Many patients are under the impression that a diagnosis of Diverticulosis means you can’t have nuts, seeds or corn in your diet. That is TRUE in a very small number of patients. However, most patients can keep these in their diet with balance and moderation. Scientific studies have been performed looking at this very point. A two-decade old study at Harvard Medical School found the patients who consumed these foods actually had a 30% decrease in the risk of Divericulitis and bleeding!
So, enjoy a balanced, high-fiber diet! What is that? It’s what my 6th grade science teacher, Mrs. Cook, told me a half a century ago. “Take a look at your plate. If there are plenty of colors and shapes, then that’s a balanced diet.” Brilliant.
James J. O’Mailia, M.D., P.A.
1553 Matthew Dr, Fort Myers, FL 33907
(239) 275-3695
 Southwest Florida's Health and Wellness Magazine Health and Wellness Articles
Southwest Florida's Health and Wellness Magazine Health and Wellness Articles

