Michael J. Petrocelli, D.P.M., F.A.C.A.S., C.W.S.P.
Foot problems most often happen when there is nerve damage, also called neuropathy. This can cause tingling, pain (burning or stinging), or weakness in the foot. It can also cause loss of feeling in the foot, so you can injure it and not know it. Poor blood flow or changes in the shape of your feet or toes may also cause problems.
The foot is especially affected by diabetes because:
• Diabetes damages the nerves (damage can occur to the foot and not be detected) – this is called peripheral neuropathy.
• Diabetes also effects the circulation. Poor circulation can affect the ability of the body to heal when damage occurs.
• Those with diabetes are more prone to infection – the body’s processes that normally fight infection respond slower and often have trouble getting to infections due to the poor circulation.
• Diabetes can also affect the joints, making them stiffer.
• Other diabetes complications that can also affect the foot, for example, kidney disease (affects proteins that are involved in wound healing) and eye disease (can’t see the foot to check for damage).
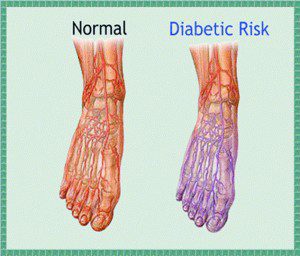
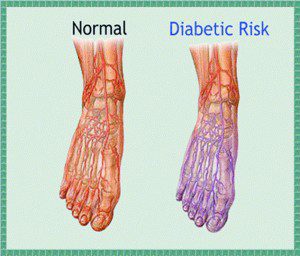
Diabetes and Poor Circulation
Our circulatory system covers a lot of ground. If our vast network of veins, arteries, and tiny capillaries were straightened and laid end to end, it would stretch more than 60,000 miles! When blood is pumped from the heart to our extremities, it can be considered quite the journey there and back. This can be especially true for blood traveling to our feet, which has both distance and gravity to deal with. When complications from diabetes result in poor circulation, your feet can suffer from a reduced ability to heal and stop infections.
Dr. Petrocelli works closely in conjunction with vascular surgeon specialist to reinstate blood flow back to the extremities whenever possible.
Poor circulation can cause a variety of problems in the legs and feet.
While reduced blood flow can already inhibit the foot’s ability to heal from injury, diabetic symptoms can also result in nerve damage that deadens the pain or sensation when an injury happens. If a cut or sore is left undetected, it can become infected or develop into an ulcer.
In severe cases, the foot may need to be amputated. Additional symptoms can combine with the effects of poor circulation to create serious complications.
Other signs of poor circulation can be:
• Non-healing ulcers
• Absent or weak pulses in the feet or legs
• Decrease in blood pressure in the feet or legs
• Lack of hair growth on the lower legs
• Blue or purplish color in feet, especially when they’re hanging down
• Cold feet
The do’s and don’ts of foot care if you have diabetes:
If you have diabetes, there are a lot of things you need to do to prevent the problems from developing in your foot:
• Inspect your foot daily (check sores, cuts, bruises, changes to the toenails; use a mirror to look under the foot if you can not see it).
• Look after your health (loose weight; stop smoking; exercise; reduce your alcohol consumption)
• Look after your feet:
– Cut toenails straight across and never cut into the corners; use an emery board or file on sharp corners.
– Do not try to remove corns and callus yourself – see a Podiatrist for this; NEVER use commercial corncures – this is so important in those with diabetes as it is so easy to damage the skin.
• Fitting of footwear is very important. Poorly fitted shoes are a common cause of problems in the foot of those with diabetes. Some advice:
– Get your feet measured each time you buy new shoes (foot size and shape change over time).
– New shoes should be comfortable when purchased and should not need a “break-in” period.
– They should fit both the length and width of the foot, with plenty of room for the toes.
– Avoid shoes with high heels, pointed toes or tight around the toes (these put too much pressure on parts of the foot and can contribute to ulcers)
Podiatric treatment of the foot in those with diabetes:
Podiatrists have an extremely important role to play in the prevention and management of complications of the foot in those with diabetes. The Podiatrist should communicate this risk status to other members of the health care team. Advice should be given on how to reduce the chance of damage happening, what to do to prevent it and what to do if something does go wrong.
Regular foot care seen by a Board Certified Podiatrist is a key way to prevent problems. The more closely you are monitored, the better your outcome will be.
Collier Podiatry, P.A.
Michael J. Petrocelli
D.P.M., F.A.C.A.S., C.W.S.P.
239-775-0019
www.collierpodiatry.com
 Southwest Florida's Health and Wellness Magazine Health and Wellness Articles
Southwest Florida's Health and Wellness Magazine Health and Wellness Articles
