By Ellen Poage, MSN, MPH, FNP-C, CLT-LANA –
Lymph system failure can occur in children either at birth or in adolescence because of a genetic predisposition to a weak or insufficient lymph system.
A type of parasitic infection can also block the lymph system resulting in 3rd stage lymphedema, or elephantiasis. This is common in countries like Haiti and India.
Here in the United States lymphedema is commonly related to venous insufficiency or else is triggered by lymph node dissection as a result of cancer surgery and radiation. The lymph system transports protein rich fluid from the tissues back to the heart where it returns to the blood circulation. The lymph system’s main function is not to return fluid but particles, proteins and debris that are essential for healthy circulation and immune function.
On the other hand, the venous system’s main function is to return fluid back to the heart but it cannot reabsorb the proteins or larger particles.
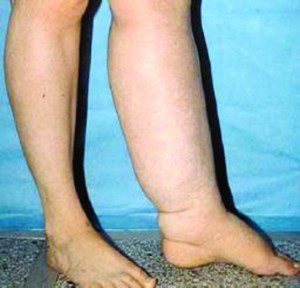
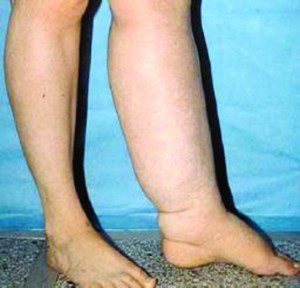
If the veins wear out, due to age, inactivity, prolonged standing or sitting, the legs will swell because the fluid is not returning to the heart. In the case of venous insufficiency the lymph system can help temporarily when the veins start to fail by increasing their workload. This is not meant to be permanent so eventually this added workload causes a lymph transport failure. You will see pitting edema in the leg, meaning a dent forms when you press your finger in the tissues.
At this point your physician may prescribe a diuretic. The diuretic can remove the fluid from the tissues by increasing reabsorption of fluid into the veins but the protein particles remain. Often the diuretic makes the situation worse because it pulls the water leaving condensed proteins in your tissues.
If you have ever wondered why the benefits of a diuretic are temporary it’s because water loves protein so where protein goes water follows. Think of dry beans in a pot. When you put water in the pot, the beans swell.
You may have noticed elevating the limb helps early in the disease process but after a while this no longer works because as lymphedema progresses, the stagnant fluid and proteins eventually become fibrotic, otherwise known as scar tissue. Fibrosis is an inflammatory process that causes the skin to thicken, fatten and harden. This interferes with joint mobility making it difficult to walk or in upper extremity lymphedema, difficult to bathe, groom or dress.
In addition to disease progression with fibrosis, bacteria love proteins. A small break in the skin can lead to infection or cellulitis resulting in hospitalization if not treated early.
Therapy Options
If lymphedema develops, it is essential to seek the help of a certified lymphedema therapist without delay. Timely referral can help prevent infections, fibrosis, loss of function and quality of life. The importance of early detection and treatment cannot be overemphasized. Lymphedema is a disease treated with physical therapy called Complete Decongestive Therapy (CDT). Lymphedema is not always reversible but it can be managed. Often people are given an intermittent pneumatic compression device as first line of therapy. Although there is a place for the use of pumps for lymphedema, they should not be the first intervention.
Complete Decongestive Therapy:
Therapy begins with a comprehensive assessment that includes measuring the area of swelling. CDT is an intensive four-step process that takes about 2 to 3 weeks. Each visit consists of manual lymphatic drainage (MLD), compression bandaging, skin care and exercise. MLD is a form of manual therapy that stimulates the lymphatic system to move lymph fluid. Compression bandaging encourages the continued flow of lymph and decreases the return of lymph. These are worn daily. While highly effective, bandaging is challenging because wraps are worn daily and it requires learning the technique and is time consuming. All four steps are continued in self-care. Self-care is ongoing.
Self-care is essential to managing lymphedema. During self-care the all day bandages are replaced with a fitted compression garment and if needed nighttime wraps are used.
While lymphedema therapy is more available today, there are few trained and skilled therapists. Be prepared to inform your health care provider of your symptoms and if you are not getting results from therapy, be prepare to find a new therapist. One thing is certain, though: if you manage lymphedema it will not manage you.
Lymphedema Therapy is available locally at 8660 College Pkwy., Ste. 60, Ft Myers. For more information, you may contact Associates in General & Vascular Surgery, a division of 21st Century Oncology, at (239) 939-2616.
Ellen Poage, MSN, MPH, FNP-C, CLT-LANA is a family nurse practitioner with Associates in General and Vascular Surgery. She is a Certified Lymphedema Therapist with the Lymphedema Association of North America. She lives in Fort Myers and has been treating lymphedema since May 1995.
 Southwest Florida's Health and Wellness Magazine Health and Wellness Articles
Southwest Florida's Health and Wellness Magazine Health and Wellness Articles

